A few months ago, Ashley Gulsby was helping her mom clean a bedroom for a housekeeping client when she noticed a copy of the local paper on a nightstand. There it was in bold black letters: “Grove Hill Memorial Hospital ending labor and delivery services.”
The hospital in Grove Hill, Alabama, an 1,818-person town at the crossroads of two regional highways, was never anything big—there are only 19 beds—but to Gulsby, it was the “pride of the town.” Her mother had given birth to her in one of its three delivery rooms, and 20 years later, she had her first baby there. She had always assumed that her second baby, a boy due in September, would also be delivered at Grove Hill Memorial.

“I was not happy,” said Gulsby, 34. “I don’t want to be birthing a child in the back of no vehicle.”
Just a week earlier, at 35 weeks pregnant, Gulsby went to Grove Hill Memorial for a checkup. Now, she would have to travel an hour and a half to a hospital outside Mobile at the first sign of a contraction.
“God forbid something goes wrong,” said Gulsby, a former ambulance dispatcher. “Babies don’t wait for nobody.”

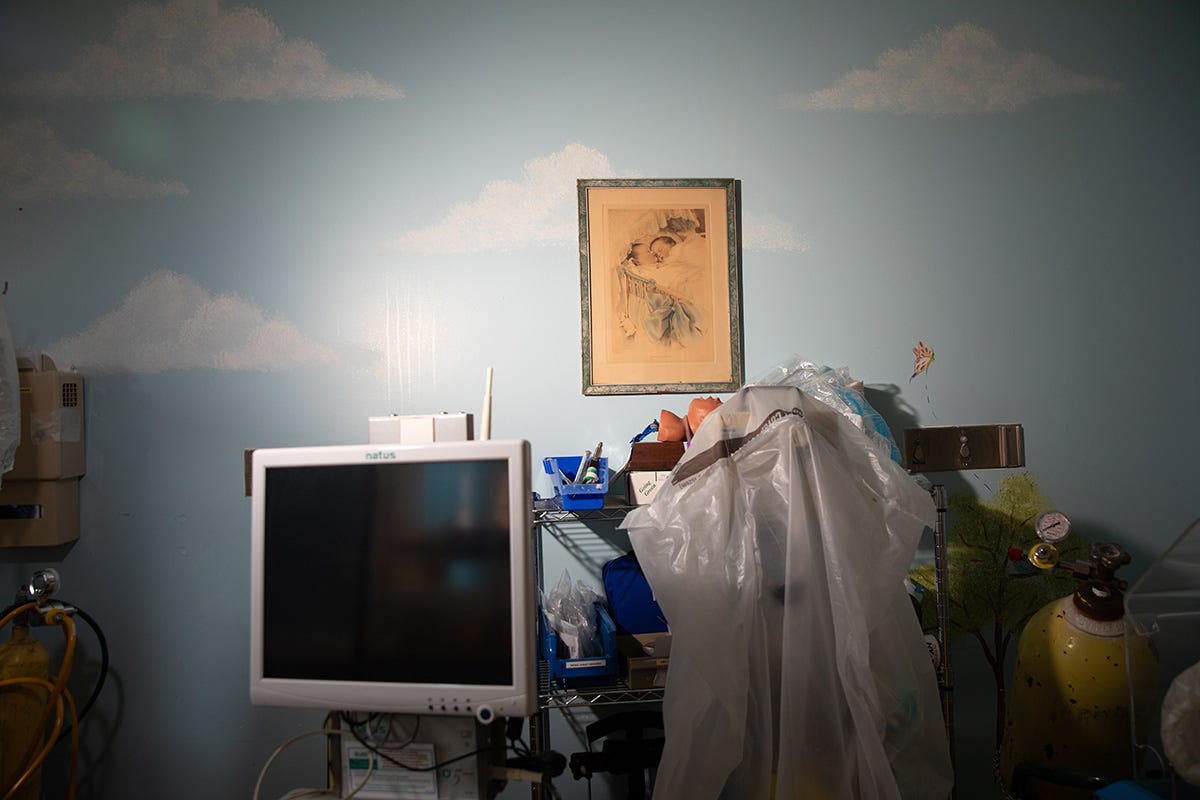
Sure enough, at 7 p.m. on August 16, Grove Hill Memorial Hospital shut off the lights in its ob-gyn unit, becoming the fourth hospital in Alabama to shutter its maternity ward in just under a year. The closures have created a vast maternity-care desert in the state’s southwest corner. Women in Clarke County—where Grove Hill is the county seat—now have to drive some of the farthest distances in the nation if they want to give birth in a hospital.
Across the U.S., rural hospitals are struggling to stay afloat, with many slashing unprofitable labor and delivery units. The trend is driven in part by declining birth rates in rural America—Clarke County, for instance, has experienced a 41 percent drop in annual births since 1990. But it’s also because the majority of rural patients use Medicaid as their health insurer. And Medicaid’s reimbursement rates are punishingly low.
Like so much of rural America, Grove Hill has been hollowed out since the 1980s. So has nearby Jackson, almost 20 miles to the south, another town whose hospital no longer has a maternity ward. Dr. Sid Crosby, who delivered babies in Jackson from 1984 till 2012, said that he and his wife were first attracted to Jackson because of its vibrancy.
“It was a rural town, but it was a young town,” he told me. “We saw kids playing. You know, most rural towns are old—the young people are moving away. What impressed us is that Jackson seemed different.”
Crosby added: “Unfortunately, what’s happened to Jackson is like what’s happened to most rural areas.”
Kristina Anderson, a 27-year-old mother of three who grew up in Jackson, agreed. There “used to be a lot more going on,” she said, speaking to me during a lunch break from her customer-service job. “We used to have a theater. There used to be a lot more to do here for kids.”
But in the 1980s, Clarke County began its slow decline. When Walmart came to town in 1999, it put the downtown stores out of business. The independent grocery became a Pentecostal church; the auto-parts retailer became a funeral home. Nine public schools became seven.
But there were always the hospitals. However relentless the decline of the two towns, at least you could get real medical care.
“That was about the last good thing we had here,” Gulsby said in a whisper. “There is no future for Grove Hill now.”

On a Sunday in August, a week before Grove Hill Memorial closed its maternity ward, I watched Allen Jordan, the hospital’s interim CEO, perform his morning routine: flipping through the hospital’s list of debtors to see who he could pay first.
“We owe most everybody that we use,” he said, raising his eyes from the spreadsheet. I took a peek: $564.13 to FedEx; $30,588.08 to Cardinal Health, the big medical supply distributor; $1,032 to Computer Programs and Systems, Inc.
“We have asked for extensions,” Jordan said. “People have given us all the leeway they’re able to give us. Now we’re in a pretty tight credit crunch, living insurance reimbursement to insurance reimbursement.”
Staff at both Grove Hill Memorial and Jackson Medical Center told me Medicaid reimbursements didn’t even cover their costs of labor and delivery—Jordan said that Medicaid reimburses an average of $1,800 per birth, even though the procedure usually costs the hospital $5,600. Crosby said that as many as 80 percent of Jackson Medical Center’s patients were Medicaid recipients.
“The hospital was driving it, saying, ‘Look, we just can’t afford to pay these nurses, anesthetists, and all the staff to keep doing obstetrics when we’re not getting paid enough to justify it,’ ” Crosby said.

Jordan told me that when he stepped in as CEO in July, he inherited the “heavy burden” of righting the hospital’s finances. One of the first things he did was print out more than a hundred letters on official stationery—one for each vendor—thanking them for their patience. Had he gotten any replies?
“Not yet,” he said, toying with a paper clip.
The hospital’s debts, Jordan said, feel like his own. “There’s no more help coming,” he said. “There’s no more Covid money coming. There’s no more tax relief. There’s nothing else coming.”
Closing its maternity unit was Grove Hill Memorial’s way of doing something different. That’s because in early 2023, the Centers for Medicare and Medicaid Services established a program to pay individual hospitals more than $3 million in annual federal aid if they agree to keep their average patient stay under 24 hours. In practical terms, this means that the hospitals have to shut down everything besides their emergency units to be eligible for the money. Grove Hill Memorial’s application is still pending, but if it is approved, the hospital will get a lifeline of $261,333 a month. With that kind of cash, Jordan figures that the hospital, which lost $1.6 million last year, could become profitable within six months.
“We either have to do something different, or we won’t exist anymore,” Jordan said.

No one in Clarke County is blaming Jordan and other hospital administrators for the closing of the ob-gyn unit. They understand the dilemma—you can’t keep a maternity ward open if there aren’t enough babies to sustain it or enough money to pay for it.
What many residents don’t understand is why the state government won’t step in. Especially a state government like Alabama that professes to be pro-life and has gone to extraordinary lengths in the wake of the Supreme Court decision to overturn Roe v. Wade to prevent abortions from taking place on its soil.
To Dr. Max Rogers, who had been one of two delivering physicians at Grove Hill, the consequences of these closings are going to be dire.
“Babies are going to die, and mothers are going to die,” he said.

Jessica Overstreet, a 33-year-old expecting her fifth child, told me that she realizes there was “no easy answer to keeping the doors open” at Grove Hill Memorial. “I understand there’s no such thing as a free lunch,” she said, standing outside the farmhouse she and her husband built. “But when you have people in a position of power that stand up there and say they’re pro-life when they put mothers and babies at risk, it’s complete hypocrisy.”
“I feel forgotten. I feel forgotten by our lawmakers,” added Overstreet. “I have two daughters—I worry about what’s going to be here for them.”
When Overstreet was pregnant with her eldest, now 11, she was studying at the nursing college in Monroeville, about an hour away. That’s how she ended up giving birth to her first child at the Monroe County Hospital. Happy with the care she received at the hospital, she went to Monroe County for her next three deliveries. But four years ago, during the labor of her last child, she nearly went into septic shock. Like millions of women, Overstreet carries a gut- and genital-based bacteria called Group B strep, which can be harmful to both mother and baby. When she felt contractions coming, she and her husband raced to Monroeville.

“We barely made it in time,” she said of the hour-long drive. “My husband had to lift me up out of the truck and put me in a wheelchair, and I actually delivered in the wheelchair.” She ended up spending five days in the ICU—a crisis she said could’ve been avoided if she had made it to the hospital in time to take antibiotics before entering labor. (Monroe County Hospital has since closed down its maternity ward, along with its inpatient services, as it also attempts to be accepted into the same federal program as Grove Hill Memorial.)
Overstreet was 17 weeks pregnant with her fifth child when we met. She had planned to have her baby delivered at Grove Hill Memorial, which is only 25 minutes from her home. Now that option is gone. “It’s just scary because I’ve got all these kids that depend on me. I have a husband, and we’re a family unit, but at the end of the day, they need a mom, too.”
One politician locals blame for the closure of their maternity-wards is Alabama governor Kay Ivey, whose pro-life credentials include signing the strictest abortion bill in the country in 2019, making it a felony to perform an abortion with no exception for rape or incest. The law was on hold while Roe v. Wade was the law of the land, but three years later, the Supreme Court overturned it, ruling that abortion was an issue for the states. That caused the Alabama law to go into effect, as well as similar laws in nearly two dozen states.
In the handful of states that held referendums on abortion, the pro-life side has consistently lost. Yet some 13 states now have pending bills that go even further, including bills that would treat frozen embryos as children. This latest move was sparked by an Alabama state supreme court ruling in February that fertility clinics could be prosecuted for destroying embryos. (The Alabama legislature quickly passed a law to protect these clinics.)
In Jackson, I met Johnny Kendrick, the lead pastor of the Tompkins Baptist Church and a staunch pro-life advocate. After his Sunday service, we spoke in his office. I asked him how he felt about the fact women in the area now have to drive nearly 80 miles to deliver a baby.
He leaned back in his leather rolling chair for a second, then told me, “To say you’re pro-life, and then not fund the healthiest outcomes for children, is a little hypocritical.”
Was he frustrated with the state’s leadership? I asked.
“That’d be a fair statement,” he said. “I wish that they would do things differently.”

Anderson, the 27-year-old mother of three, told me that when she was born, she was one of the first babies delivered by a new doctor at Jackson Medical Center.
Now her newborn son carries the reverse distinction—the last baby ever born in Grove Hill Memorial. Malakai was delivered at 2:44 a.m. on August 16, the day Grove Hill closed its maternity ward. He came out with a single push, she said—just like her other two kids. “They come real fast,” she added. “No time for an epidural, no pain medicine.”
Anderson and her husband want another child. She said she’s taken the issue to God recently, praying whenever the feeling hits her, whether it’s at the kitchen sink or while changing Malakai’s diaper, to ask for a new obstetrics doctor in town.
“What can you do but just pray and take it day by day,” Anderson said. “I mean, there’s nothing you can do to make a change, because we’re not the governor. Nobody’s going to listen to us. What can we do?”
She said she doesn’t see herself making the hour and a half trek to Mobile to deliver her next baby, but at the same time, she still wants to grow her family.
“This is my body and I should be able—with God’s will—to carry as many children as I and God would like,” Anderson said. “I don’t feel like it’s fair.”
Olivia Reingold is a reporter for The Free Press. Follow her on X @Olivia_Reingold and read her piece, “Addiction Activists Say They’re ‘Reducing Harm’ in Philly. Locals Say They’re Causing It.”
Real reporting across America takes time and resources. To support our independent journalism mission, become a Free Press subscriber today:









our Comments
Use common sense here: disagree, debate, but don't be a .