
The Free Press

What do you do if you are the parent of a child who believes they were born in the wrong body? What if your kid doesn’t fit the stereotypical behavior of their sex—your daughter is a tomboy, your son is effeminate—and a teacher or school counselor suggests they might be transgender? What if your teenager, uncomfortable with their changing body at puberty, says they will harm themselves—or worse—if they are not allowed to medically transition?
A growing number of parents are facing such questions in 2022. Desperate for answers, they are turning to the experts: the doctors, psychologists, and professional organizations devoted to diagnosing and treating gender dysphoria.
Among the most important of these associations is the World Professional Association for Transgender Health (WPATH). Founded in 1979, it is regarded by many as a premier advocacy group for medical care, education, and research regarding transgender and “gender diverse” people. Though it’s not a medical association—in addition to doctors and psychologists, its ranks include lawyers, educators, students, and electrologists—WPATH’s Standards of Care are considered by practitioners around the world to be the gold standard of recommendations for treating gender-related distress.
WPATH has just released a long-awaited update to those Standards of Care for people seeking “lasting personal comfort with their gendered selves.” This 260-page update— the eighth version of WPATH’s standards—includes several new chapters. One is on the increasing number of nonbinary individuals. A second is on supportive care for “those who identify as eunuchs” and “may also seek castration to better align their bodies with their gender identity” (yes, you read that right). A third, and perhaps the most anticipated, is on the treatment of transgender of gender diverse adolescents—added, writes WPATH, due to “the exponential growth in adolescent referral rates.”
This skyrocketing population of young people with gender dysphoria is fueling our culture wars. Some states, including Alabama and Arizona, have outlawed gender medical treatments of minors—including irreversible hormonal and surgical interventions—while other states are seeking to make it a felony to provide such care. In response, California aims to pass a law to become a sanctuary state for minors seeking gender medical interventions—even without parental consent.
Controversies have surrounded some of the country’s leading children’s hospitals, due to the young ages at which they offer life-altering surgeries—such as double mastectomies for girls, and surgeries for older teens that will permanently sterilize them. (These surgeries include vaginoplasties—the removal of penis and testicles and the creation of a neo-vagina from that tissue—for males, and hysterectomies for females.) Boston Children’s Hospital received a bomb threat after videos it made promoting its surgeries for young people were shared on Twitter. In another incident, the Transgender Health Clinic at Vanderbilt University Medical Center took down its entire website after a leaked video went viral. The video featured one of the clinic’s physicians describing how these surgeries have become “huge money makers” and that in some cases, an “entire clinic is supported just by the phalloplasty.”
To calm this strife, WPATH could have produced an evidence-based, apolitical document for physicians and others desperately seeking guidance. That’s not what happened.
The new guidelines are “a weird amalgam of pseudo-medical speech, and political statements, and fetishistic practices,” said Julia Mason, a pediatrician in Oregon and a clinical advisor to the Society for Evidence-Based Gender Medicine. Dr. Mason added that she was dismayed that WPATH rejected the chapter on ethics that had been in an earlier draft, but retained the chapter on eunuchs. (These guidelines see eunuchs not as a deeply tragic part of history but as a “gender identity” which health care professionals should support.)
The rollout of these new Standards of Care has been marred with confusion. Last December, WPATH released draft guidelines, which included minimum age recommendations for life-changing treatment, including age 14 for receiving estrogen or testosterone (the previous WPATH standards had been age 16), and allowing minors to have mastectomies (which the guidance often calls “chest-masculinization surgery”) beginning at age 15, and vaginoplasty and hysterectomy at 17.
The official guidelines were then released online to the public September 15. Within hours, a major correction was appended that said that the recommended age minimums were being removed from the final document. It turns out that between the draft release and the final version, WPATH had backtracked on providing age minimums, preferring to leave decisions to practitioners.
Why the reversal on such an important issue? WPATH is notoriously resistant to the press (the organization has not responded to my request for comment), and has offered no official explanation. But on Monday, The New York Times quoted WPATH President Marci Bowers—a surgeon who is herself transgender—as saying that reinstituting the young age recommendations will require “a better political climate.”
Then came a video from the WPATH annual conference last week that was posted on Twitter.
In the video, Amy Tishelman—a psychologist at Boston Children’s Hospital and the lead author of the WPATH chapter on children—discusses why the chapter on children was vaguely worded. “We were thinking, and it was scary for me, about the potential uses of the chapter for legal and insurance contexts,” Dr. Tishelman said. “What we didn’t want to do was create a chapter that would make it more likely that practitioners would be sued because they weren’t following exactly what we said.”
After an uproar, WPATH put out a statement claiming that the video “was taken out of context, twisted and used to spread hate and lies on social media.” It added that Dr. Tishelman was talking about “therapeutic support” and “not medical care.”
James Cantor is a psychologist and sex researcher in Toronto who has for years analyzed the research on treating kids with gender dysphoria. He told me that the updated standards of care provide a “collective shield” so that gender clinicians can do whatever they want and “call it professional judgment.” He added: “The current version is written in so much couched, vague, and contradictory language that essentially I think it's become hard to interpret this as anything other than a Rorschach test, to which anybody can say whatever it is they want to say, and this will be the coverage they need to justify doing whatever it is they want to do.” He said the goal of the standards was clear: “This was made to protect the doctors from lawsuits. None of this has ever been about patients."
A prime example of the lack of concern about kids: WPATH recommends that “in almost all situations, parental/caregiver consent should be obtained,” except “when caregiver or parental involvement is determined to be harmful to the adolescent.” But who determines what “harmful” is? And does it simply mean not giving the child what they want?
One WPATH author even suggested at the group’s conference that practitioners could call Child Protective Services on parents reluctant to transition their kids. Such weaponizing of CPS has happened both to parents who oppose their child being transitioned—as I have documented—and to parents who facilitate it.
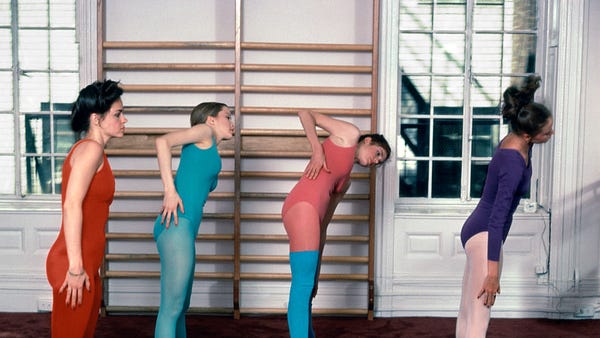
When the last WPATH guidelines were published in 2011, the phenomenon of adolescents—overwhelmingly female—suddenly declaring themselves to be transgender was rare. But in the past decade, across the Western world, many countries have seen an exponential increase in this patient population of teen girls. Britain has experienced a more than 4,000 percent increase.
These are the kinds of young female patients with multiple mental health disorders that psychologists have been treating for years. Often these patients are dealing with anorexia, and engaging in cutting and other self-harm. But now, rather than partaking of talk therapies, they often end up being affirmed in their new gender identity, and are sometimes sent down the pipeline to medicalization—their other mental health issues ignored.
Cantor observes that now these girls aren’t just cutting their own arms; they are getting surgeons to cut off their breasts. The young people showing up at gender clinics are genuinely distressed, he said to me. “They actually do need meaningful help, but they’re not getting help for the problems they have. They’re getting help for the problems they say they have.”
As I wrote in a previous article for Common Sense, medical establishments in some European and Scandinavian countries have noticed the explosion in this population and have undertaken systematic reviews of the science on youth transition. They came away alarmed at the low quality of evidence supporting the efficacy of youth medical transition, considering how little is known about the potential side effects of these treatments—including osteoporosis, delayed brain development, sexual dysfunction, increased risk of cancer and other diseases. They also found that detransition and regret about transition were higher than expected.
In response to these reviews, these countries have variously put restrictions on medically transitioning young people. They now recommend that dysphoric children and adolescents get careful mental health evaluations, and that psychological support should be the first line treatment, with the goal of exploring the many psychological and social reasons for their feelings.
Of course, the WPATH writers had access to the same universe of information as the Europeans and Scandinavians. They acknowledge that “a key challenge in adolescent transgender care is the quality of evidence evaluating the effectiveness of medically necessary gender-affirming medical and surgical treatments.” But instead of being concerned by the paltry evidence, WPATH has falsely claimed that “a systematic review regarding outcomes of treatment in adolescents is not possible.” They also declare puberty blockers are “fully reversible”—but we simply don’t know their long-term impact. They reject the cautionary principle employed by other countries, and leave decisions to individual doctors and patients for any treatment—social transition, hormones, surgery.
The long-term effects of these interventions on the kinds of adolescents seeking them today is unknown, but WPATH notes positively that a “2017 study of 20 WPATH-affiliated surgeons in the US reported slightly more than half had performed vaginoplasty in minors.” Yet some detransitioned men who received vaginoplasties are speaking out, saying they realized they were gay men with internalized homophobia—and that they weren’t properly evaluated before having their genitals removed.
Decades of studies, and experience by practitioners, demonstrate that the vast majority of children with early-onset gender dysphoria outgrow this by the time they emerge from puberty—and that many of these young people grow up to be gay or bisexual. WPATH even acknowledges that “there are no reliable means of predicting an individual child’s gender evolution.” So by promoting the benefits of early social and medical intervention, WPATH advocates preventing the very process of natural physical and mental maturation that has historically resulted in the resolution of most dysphoric children’s distress.
Parents desperate to care for their children need recommendations based on a systematic review of the evidence—recommendations that take into account the changing demographics of gender-distressed teens and the emerging cohort of detransitioners. Practitioners, medical associations, parents, and, most of all, people with gender dysphoria deserve nothing less.










what has happened here , no idea what happened to substack ?
'The video featured one of the clinic’s physicians describing how these surgeries have become “huge money makers” and that in some cases, an “entire clinic is supported just by the phalloplasty.” '
How about a piece reporting on how much of catering to end of life veterinary care pays the bills?
Seems much the same, albiet with far lower stakes, than the folks whose 14 year old gets caught up in this and can’t find the will to say, "no."
Always another chargeable medical procedure available.
Animals on dialysis and chemotherapy. Squeaking out a few more months of existence is somehow easier for the owners who won't choose pre-emptively, to put an aged pet down.